A damning report has revealed that staff at HMP Wandsworth failed to provide adequate CPR to a prisoner experiencing cardiac arrest, with significant delays in emergency response and substandard resuscitation efforts.
Systemic Failures in Emergency Response
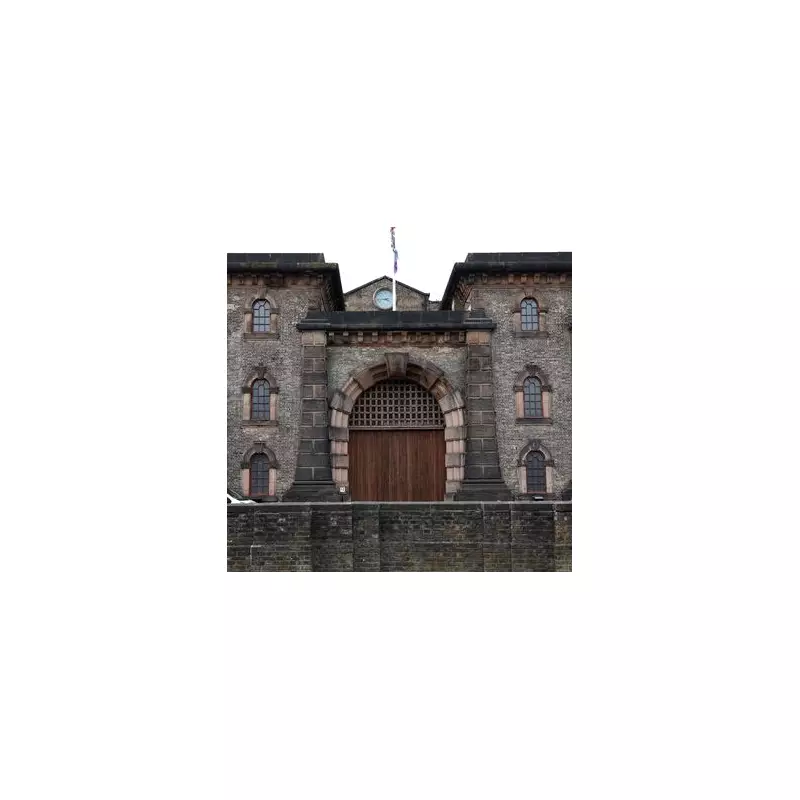
Peter Honnor, 55, died of myocarditis at the South London prison on June 27, 2024, after his cellmate reported him unresponsive in the early hours of the morning. The Prisons and Probation Ombudsman investigation found that the night patrol officer did not immediately declare a code blue emergency, causing critical delays before other officers arrived, opened the cell and summoned an ambulance.
Paramedics who eventually attended the scene raised serious concerns about the quality of resuscitation performed by both healthcare and prison staff before their arrival. Their assessment revealed multiple deficiencies in the emergency response.
History of Medical Concerns Ignored
Mr Honnor had been remanded in custody to HMP Wandsworth on May 6, 2024, for threatening a person with a blade in a public place. He had a documented history of heart attacks and heart failure, and was seen repeatedly by healthcare staff during his short time in prison.
Medical records show he experienced chest pain, dizzy spells and at least three falls - two of which resulted in head injuries. He was admitted to the prison healthcare unit on May 23 where his blood pressure was monitored twice daily.
On June 18, Mr Honnor requested an appointment because he felt like he was going to pass out. He was placed on the GP waiting list for June 25, but there is no record he actually saw a doctor.
Missed Opportunities for Intervention
The investigation uncovered several concerning incidents in the days leading up to his death. On June 22, prison staff called a code blue emergency after Mr Honnor blacked out and fell against a cell wall. By the time staff assessed him, he had returned to normal and no further clinical intervention was made.
Critically, the fall was not discussed with a doctor and there is no evidence that consideration was given to sending him for a CT scan. Just three days before his death, a nurse recorded that Mr Honnor was "well."
Final Hours and Resuscitation Failings
At approximately 4:18am on June 27, Mr Honnor's cellmate alerted a night patrol officer that he was not breathing. The officer called for help but failed to radio a code blue emergency, and later told investigators he couldn't enter the cell because he wasn't carrying a mandatory cell key.
When other officers and healthcare staff eventually arrived and began CPR, their efforts were described as inadequate by paramedics who later took over. The emergency medical team noted that chest compressions were performed at insufficient depth and excessive speed, defibrillator pads were incorrectly placed, and oxygen was not administered.
A nurse involved in the resuscitation told the ombudsman that healthcare staff failed to provide effective leadership during the emergency and their approach did not comply with established guidelines.
Clinical Review Findings
The clinical reviewer determined that Mr Honnor did not receive the standard of care he could have expected in the community. While acknowledging that successful resuscitation was unlikely given his heart had already stopped, she emphasised that CPR should always be performed according to established guidelines.
The review also found that healthcare staff stopped investigating Mr Honnor's low blood sodium levels after changing his medication, without considering other potential causes or whether his heart failure was progressing. A more structured approach to investigating his condition, including a case review, should have been implemented.
Following an inquest that concluded on September 12 this year, a coroner confirmed Mr Honnor died of natural causes.
The ombudsman has instructed the prison's governor and head of healthcare to thoroughly investigate the events of that night and the concerns raised by paramedics. They must identify learning opportunities and develop an action plan for staff improvement as necessary.
Oxleas NHS Foundation Trust, which provides healthcare services to HMP Wandsworth, has been contacted for comment regarding the findings.





