The government has unveiled an ambitious £170 million action plan to eliminate new HIV transmissions in England by 2030, with groundbreaking measures including the ability to order HIV test kits through the NHS app and routine opt-out testing in emergency departments.
Groundbreaking HIV Prevention Programme
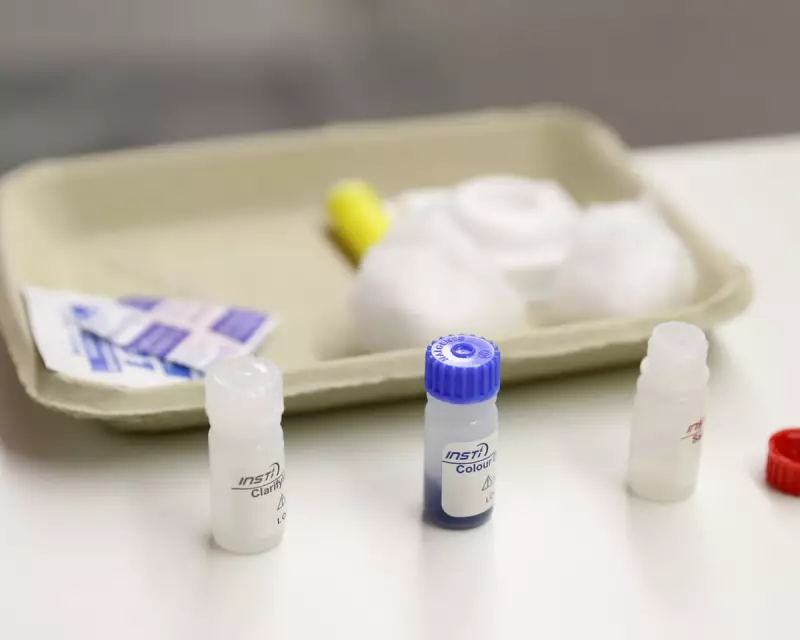
Prime Minister Keir Starmer announced the comprehensive strategy, which represents the most significant investment in HIV testing and care in decades. People will be able to order HIV test kits directly through the NHS app, providing a discreet alternative to clinic visits for those anxious about their sexual health.
The plan, to be launched on World Aids Day, includes a £5 million trial for the new digital service that aims to make testing more accessible. Health Secretary Wes Streeting emphasised that ending new HIV transmissions by 2030 is an ambitious but achievable goal, noting that today people living with HIV can enjoy full, healthy lives and cannot pass the virus to others when receiving proper treatment.
Expanding Testing Through A&E Departments
A crucial component of the strategy involves implementing opt-out HIV testing during routine blood tests at A&E departments in areas with the highest HIV rates, including London and Manchester. This approach has been described as "transformational" by health experts.
Richard Angell, chief executive of the Terrence Higgins Trust, stated: "The government has an ambition that is both momentous and historic: that England becomes the first country in the world to end new HIV cases. This new plan recognises the scale of the challenge."
Hospital staff in trusts where the opt-out scheme operates will receive anti-stigma training, ensuring patients can access care without fear of judgment regarding their HIV status.
Re-engaging Vulnerable Populations
The action plan specifically targets the approximately 5,000 people living with HIV who have fallen out of medical care, according to a National AIDS Trust report published in September. The Department for Health and Social Care identified multiple reasons for this disengagement, including mental health issues, addiction, poverty, and fear of judgment.
Professor Susan Hopkins, chief executive of the UK Health Security Agency, highlighted both progress and remaining challenges: "About 95% of those living with HIV now know they have the virus. But about 4,700 people remain undiagnosed, including one in three in Black African communities and higher rates of late diagnosis in older age groups."
She stressed the need for testing that "meets people where they are, in ways that feel safe and accessible."
Improving Access to Prevention Medication
The plan also addresses barriers to accessing pre-exposure prophylaxis (PrEP), a medication that can reduce the risk of acquiring HIV from sex by about 99%. While PrEP is free on the NHS through sexual health clinics, research shows it can be difficult to access in practice.
Professor Hopkins emphasised the need to "make starting PrEP straightforward for anyone who wants it, with particular focus on heterosexual and Black communities who are being failed by current disparities."
Additional measures include funding formula milk for all babies born to mothers living with HIV, as part of comprehensive HIV prevention measures for newborns.
The initiative comes at a critical time, as progress in reducing HIV diagnoses in England, steady since 2005, faltered during the pandemic due to disrupted testing and an increase in new cases. With new treatments making HIV a manageable condition, the government aims to renew momentum toward its 2030 elimination target through this comprehensive approach combining digital innovation, expanded testing, and targeted support for vulnerable communities.





