Survivors of female genital mutilation (FGM) in the UK are facing an agonising choice: fund expensive private treatment abroad or live with the lifelong physical and psychological consequences of the procedure. This is despite a World Health Organisation-approved reconstruction surgery being freely available on public health services in several European countries, including Switzerland.
The Surgical Procedures Offering Hope
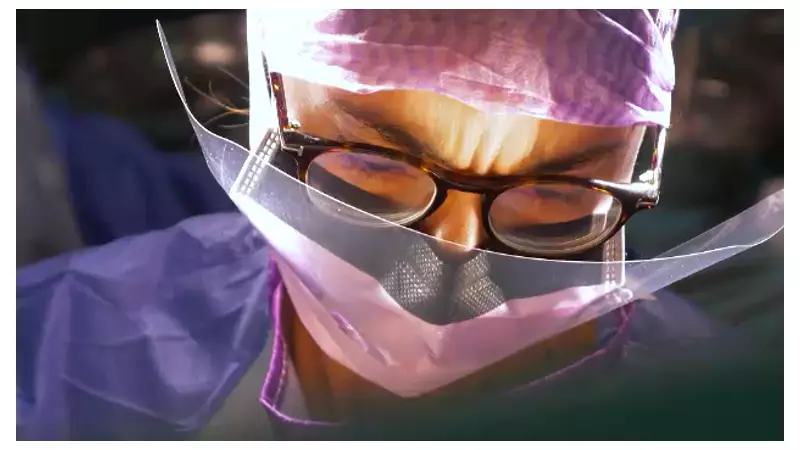
At the forefront of this medical field is Professor Jasmine Abdulcadir, one of the world's leading experts, who treats up to 30 survivors a month at Geneva's University Hospital. She explained that not every patient requires or chooses surgery, as the procedures vary depending on the type and severity of the FGM.
"If we talk about clitoral reconstruction, this is for patients that have been cut on the clitoris," Professor Abdulcadir told Sky News. "The surgery aims at removing the scar, and making the clitoris more accessible and more sensitive."
For survivors of infibulation, where the vulva has been sewn closed, a procedure called deinfibulation is performed. "When the vulva is closed, there are major obstructive complications," she explained. "It's difficult to have penetrative sex, to deliver normally. Deinfibulation allows us to open the scar. We can also reconstruct the inner labia."
A Survivor's Lifelong Trauma
The profound impact of FGM is starkly illustrated by the experience of 'Jamilla', a patient of Professor Abdulcadir who underwent reconstruction surgery just over a month ago. She recounted the horror of her childhood mutilation in West Africa more than three decades ago.
"Every girl who came in came out crying, screaming," Jamilla recalled. "I didn't want to go in, but they forced me and when I went in, she cut me with a blade. I jumped from the pain. All the girls were crying. I didn't want to, but they forced me."
Tricked by one of her father's wives under the pretence of buying sweets, Jamilla was subjected to the brutal practice. The psychological scars have persisted into her adult life. "For me, honestly, it was exhausting. I didn't want to have to heal from it... I always think about it. It's something that never leaves you. You think about it all the time."
The Scale of the Problem and the UK's Response
The World Health Organisation estimates that more than 230 million women and girls alive today have undergone FGM across Africa, Asia, and the Middle East. In the UK, a 2015 report estimated that 137,000 women and girls were living with FGM in England and Wales. Between 2015 and 2023, the NHS identified FGM in a staggering 87,575 attendances at NHS Trusts and GP practices, with the true figure believed to be much higher.
Juliet Albert, a specialist midwife who runs an FGM clinic in west London, confirmed the growing demand for surgical help in the UK. "We do find women coming to our clinic saying they want reconstruction surgery, and we have to say 'sorry, we don't offer it here'," she said. Women express a deep desire to feel whole again, with many stating, 'I want to put back what was taken away.'
Following a critical report by the Women and Equalities Committee, the government has agreed to prioritise research into the surgery. Committee chair, Labour MP Sarah Owen, stated that the research will focus on identifying areas of greatest need, with the aim of making the procedure available on the NHS "as soon as possible."
A Department of Health and Social Care spokesperson defended the current position, stating that the NHS runs FGM clinics providing healthcare and psychological support, and that they are "facilitating further research into the effectiveness of reconstructive surgery" through the National Institute for Health and Care Research.
For the thousands of survivors in the UK, this research cannot come soon enough. While the surgery cannot erase the violence or the pain, it offers a chance many feared they would never have: the opportunity to reclaim their bodies and begin healing from a lifetime of trauma.





