Rethinking Kidney Donation: Why Markets Aren't the Answer
In the ongoing debate over kidney transplantation in the UK, a recent proposal to legalise the sale of organs has sparked significant controversy. Sandra Currie, chief executive of Kidney Research UK, argues that such a move would not address the root causes of the crisis. Instead, she calls for a focus on prevention and ethical donation practices.
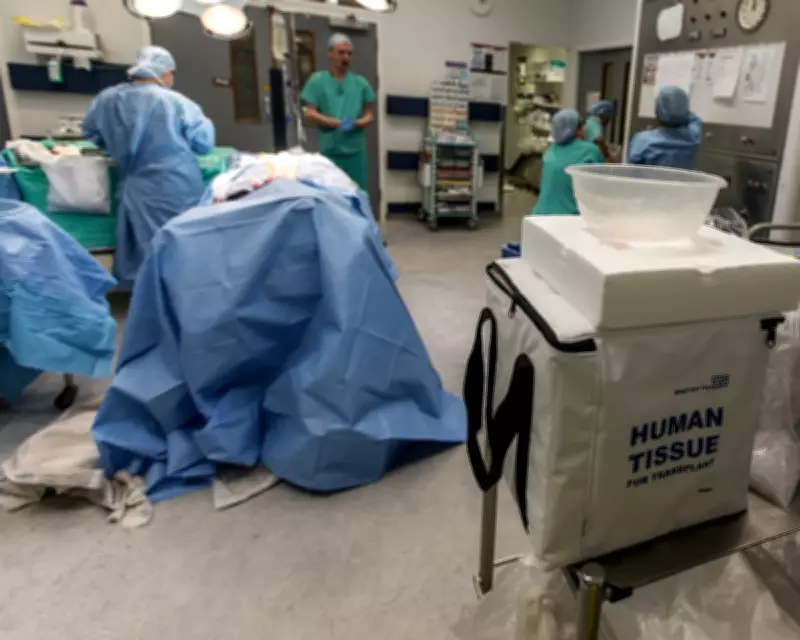
The Current Crisis in Kidney Transplants
Kidney failure remains a devastating condition, with approximately 7,000 individuals in the UK currently on the waiting list for a transplant. Tragically, six people die each week while awaiting a suitable donor. This shortage highlights the urgent need for effective solutions, but Currie warns against simplistic approaches that rely on financial incentives.
She points out that the argument for legalising kidney sales often overlooks the systemic issues within healthcare. Late diagnosis and progression to kidney failure are not inevitable; they can be mitigated through increased awareness and early intervention. By prioritising prevention, the UK could reduce the demand for transplants and save lives more sustainably.
Altruism vs. Exploitation in Organ Donation
The notion that altruism has reached its limits in the UK is challenged by recent research. Studies by the Robert Dangoor Partnership for Living Kidney Donation reveal that more than half of UK adults would consider donating a kidney to a family member, nearly a third to a friend, and one in seven to a stranger. Furthermore, over two-thirds of people express a desire to make a positive impact, even at personal cost.
Currie emphasises that the problem is not a lack of willingness to donate, but rather how effectively the system informs and supports potential donors. Kidney disease and access to care are already shaped by inequality, and introducing a market could exacerbate this by exploiting those under financial pressure. She questions the ethics of a system that depends on economic vulnerability to supply organs while ignoring underlying causes of kidney failure.
Lessons from International Examples
Dominique E Martin, a professor in health ethics, critiques the argument that markets, such as Iran's, have successfully eliminated waiting lists. She notes that eliminating a list can be achieved by restricting eligibility, but this does not solve the broader issue. In Iran, despite a legal market, only 2,500 transplants occur annually out of 32,000 dialysis patients, with concerns about exploitation and regulatory limitations persisting.
Martin highlights that the waiting list in Iran continues to grow, partly due to better patient identification and the rising burden of kidney disease. She argues that the most effective way to bridge the supply-demand gap globally is through investment in prevention and disease management, rather than relying on markets.
Challenges within the NHS Donor System
A disgruntled altruistic living kidney donor shares a personal experience that underscores systemic inefficiencies. After applying to donate, they faced a shambolic process with no follow-up, and later encountered delays when trying to help a friend in need. This anecdote reflects broader frustrations with the NHS donor system, suggesting that administrative hurdles may be contributing to the shortage of available organs.
The donor's story raises questions about whether improving support and streamlining processes could enhance donation rates without resorting to monetisation.
A Call for Ethical and Sustainable Solutions
In conclusion, saving lives does not necessitate monetising organs. Instead, it requires a multifaceted approach that includes investment in prevention, research, fair access to transplantation, and sustained support for ethical, voluntary donation. By addressing the causes of renal failure and enhancing the donor system, the UK can work towards a more just and effective healthcare framework.
As the debate continues, it is clear that engaging with reliable evidence and prioritising patient welfare over provocative proposals is essential for meaningful progress in kidney transplantation.





