The tragic death of a brilliant young man has exposed critical flaws in the NHS's right-to-choose system for ADHD patients, with experts warning of a 'wild west' in private sector assessments and a dangerous breakdown in care.
A System That Demands Stability From Those in Crisis
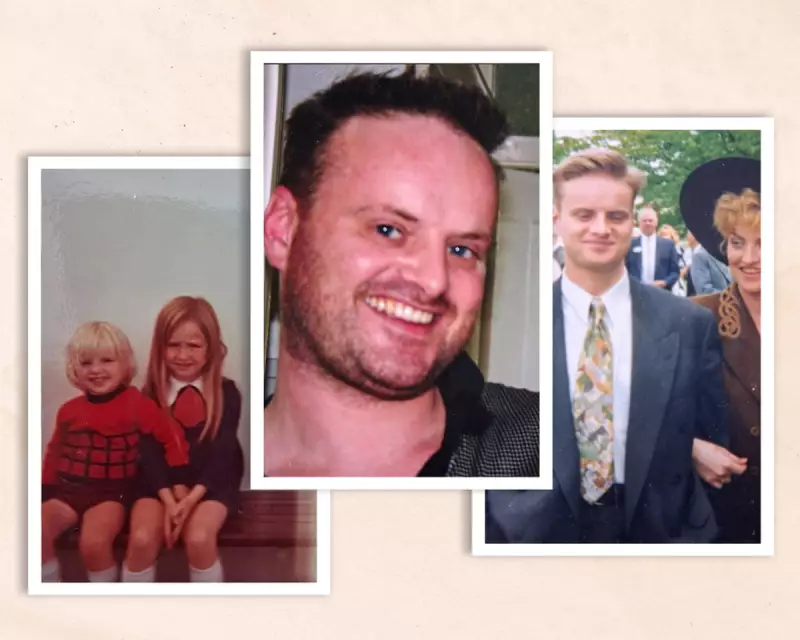
Ryan White was remembered by his sister, Leigh, as a super bright, witty, and kind individual who won five scholarships at age 11. Despite his abilities, Ryan took his own life on 12 May 2024. A subsequent report acknowledged significant failings in the support he received while seeking help for attention deficit hyperactivity disorder.
Like many others, Ryan utilised the 'right to choose' pathway, introduced in 2018 to ease decade-long NHS waiting lists. This allows patients to select a private provider for ADHD assessment and initial treatment, before requesting their NHS GP to enter a 'shared care' agreement for ongoing prescriptions.
However, Ryan became trapped in an administrative limbo. Shared care is voluntary, and not all GPs agree to it. Some patients report their private diagnoses being rejected by doctors, despite the NHS having funded the assessment and in the absence of any official standards for private providers to follow.
A Cascade of Failures and Missed Opportunities
Ryan's mental health had been deeply affected by family tragedies, including the loss of both parents. He was initially treated for bipolar disorder, but later sought clarity and was referred for an ADHD assessment with private provider Psychiatry UK in September 2022.
He was diagnosed five months later, but a community mental health review was required due to his past diagnosis, causing further delays. "Nobody chased anything, or took responsibility," Leigh White said.
By June 2023, Ryan's housing situation became unstable, triggering a rapid decline. His frustration at the delays led to him being deregistered by his GP practice. He sent desperate messages to Psychiatry UK, one of which went unanswered.
In a devastating postscript, a Psychiatry UK staff member messaged Ryan on 18 June 2024 about changing his medication, unaware he had died over a month earlier. The provider did not learn of his death until months later.
"Ryan tried so hard to get help. He was brilliant, but he was left to fall through every crack," Leigh stated. "He was fighting a system that demands stability from people who are already in crisis."
A 'Wild West' of Poor Regulation and Training
Experts argue Ryan's case is not isolated. Consultant psychiatrist Marios Adamou, founder of the UK Adult ADHD Network (UKAAN), said the right-to-choose rollout was premature, with no standard for what constitutes a good assessment or a qualified assessor.
"Right to choose was poorly regulated, poorly managed and some people are making lots of money out of it," Adamou said. "If you don't have regulation for that you are inviting a wild west."
Problems are compounded by vague assessment guidelines from the National Institute for Health and Care Excellence (NICE) and no national framework for diagnostician qualifications. Dr Jaime Craig of the Association of Clinical Psychologists said he regularly hears concerns about assessors' qualifications and assessment rigour.
Craig revealed instances where patients seeking autism assessments actually had a visual impairment, and others seeking ADHD help had language processing issues—risking incorrect medication and missing vital interventions.
Andrew Jay of North East ADHD noted NHS pressure to drive down prices leads some private providers to offer a 'very basic level of care', pressuring clinicians to be brief.
Adamou also highlighted 'aggressive promotion' by some private firms, including sharing legal letter templates with patients to pressure GPs. He warned ADHD has become 'commoditised', creating a damaging new stigma and failing those who genuinely need help.
Calls for Reform and Provider Response
Adamou has urged the NHS to halt 'uncontrolled' spending via right to choose and divert funds to NHS pathways with specific quality standards. Dr Joanne Farrow, medical director at Psychiatry UK, apologised for any part her organisation played in Ryan not getting help and said they were saddened by his death.
She stated Psychiatry UK has since invested in better safety infrastructure, evaluated policies, and opened a contact centre for faster patient responses. Their internal investigation highlighted the need for better communication with GPs and mental health providers.
Danielle Henry of the Independent Healthcare Providers Network (IHPN) said private providers now deliver over half of all NHS-funded ADHD assessments, bringing critical new capacity. She asserted members are regulated by the Care Quality Commission and adhere to clinical guidelines, but agreed problems around shared care must be addressed urgently.
The case of Ryan White stands as a stark indictment of a system designed to help, but which too often abandons the most vulnerable in a labyrinth of bureaucracy and unregulated care.





