Single Dose of Psychedelic DMT Shows Promise for Treatment-Resistant Depression
A groundbreaking clinical trial has demonstrated that a single dose of the potent psychedelic drug dimethyltryptamine (DMT), when administered alongside psychotherapy, can produce rapid and sustained improvements in individuals suffering from major depressive disorder. This finding offers new hope for the millions worldwide who struggle with treatment-resistant depression, a condition that often fails to respond to conventional antidepressants.
Significant and Lasting Effects Observed
The trial, involving 34 participants with moderate to severe treatment-resistant depression, revealed that those who received a 21.5mg intravenous dose of DMT experienced a swift reduction in depressive symptoms. These benefits persisted long after the drug's effects had subsided, with some participants reporting continued improvements up to six months later. Dr. David Erritzoe, a psychiatrist at Imperial College London and the lead investigator, emphasized the excitement surrounding these results, noting the sustained antidepressant impact from just one session embedded in psychological support.
Published in Nature Medicine, the study compared the DMT group with a placebo group, both receiving psychotherapy and follow-up assessments. The DMT recipients showed significantly better outcomes on standard depression questionnaires, highlighting the drug's potential as a novel therapeutic approach. This research adds to a growing body of evidence supporting the use of psychedelic-assisted therapies for mental health conditions.
Understanding DMT and Its Therapeutic Role
DMT is an active component of the ayahuasca brew, traditionally used in shamanistic rituals across South America. The drug induces intense, often mystical hallucinogenic experiences that can alter perceptions of time and space, dissolve the sense of self, and evoke encounters with otherworldly entities. In the context of therapy, these effects are believed to help individuals break free from entrenched, unhelpful thought patterns.
Dr. Erritzoe likened the process to shaking up snow on a mountain, flattening the landscape to allow for new pathways. This metaphorical redistribution facilitates easier navigation of mental routes, enhancing the effectiveness of psychotherapy. Unlike other psychedelics, such as psilocybin, DMT produces a shorter but more intense trip lasting about 25 minutes, which could make it more feasible for clinical settings, though it may require additional support for recovery.
Broader Implications and Future Prospects
The trial, designed and funded by Cybin UK, a neuropsychiatric firm, also explored a second stage where all participants received DMT. Interestingly, no additional benefit was observed in those who had two doses, suggesting that a single administration may be sufficient. This aligns with positive findings from psilocybin trials, which have raised hopes for regulatory approval in depression treatment later this year.
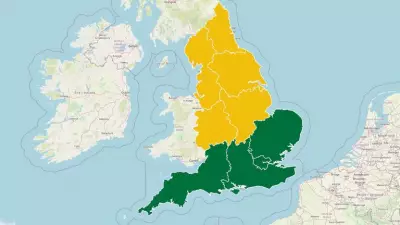
However, challenges remain in integrating psychedelic therapies into mainstream healthcare. Dr. James Rucker, a consultant psychiatrist at King's College London involved in psilocybin research, noted that if approved in the UK, these treatments might initially be available only through private clinics due to financial and stigma-related barriers. The establishment of the Feilding commission aims to guide the safe and ethical rollout of such therapies, addressing concerns over commercial pressures that could compromise patient safety.
With an estimated 100 million people globally affected by treatment-resistant depression, half of whom struggle with daily tasks, the need for innovative solutions is urgent. This trial underscores the potential of psychedelic-assisted psychotherapy to fill this gap, offering a rapid and lasting alternative for those who have not benefited from existing treatments. As research progresses, the medical community continues to explore how these powerful substances can be harnessed responsibly to improve mental health outcomes.