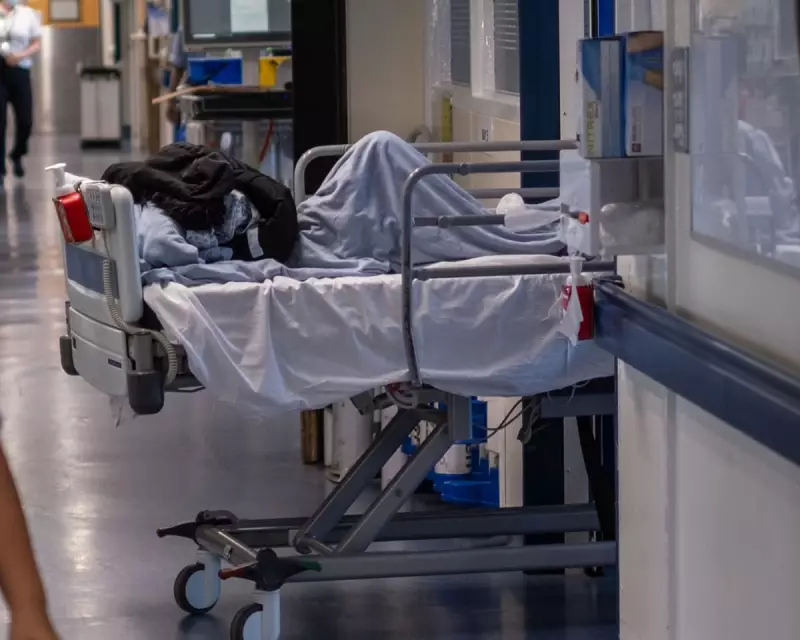
A senior medical leader has issued a stark warning that emergency departments across the UK are 'in big trouble' due to the widespread and dangerous normalisation of treating patients in corridors.
The 'Endemic' Scale of Corridor Care
Dr Ian Higginson, President of the Royal College of Emergency Medicine (RCEM), stated that the practice of caring for patients in 'escalation areas' like hallways has become so common that patients are no longer surprised by it. He emphasised that doctors simply 'can't deliver care' effectively under such conditions.
Recent analysis underscores the severity of the issue, revealing that in March, almost one in five patients in UK emergency departments received treatment in areas not designed for clinical care. Dr Higginson suspects the current situation may be even worse, reflecting a broader trend of deterioration within the NHS.
Deaths Linked to Long Waits and a Call for Action
The RCEM has previously released estimates suggesting a devastating human cost. Their figures indicate more than 16,600 deaths last year were associated with extremely long waits in A&E for a hospital bed, equating to roughly 320 fatalities per week.
"If we had 16,000 patients a year dying in bus crashes or in aircraft crashes or anywhere else there would be such howls of outrage something would be done about it," Dr Higginson told PA Media. He expressed frustration at the lack of "determined action at the highest level" in response to these statistics.
Political Pledges and Proposed Solutions
In early December, the new Health Secretary, Wes Streeting, pledged to end corridor care in hospitals in England by the next general election, "if not sooner". A Department of Health and Social Care spokesperson echoed this, calling the situation "unacceptable and undignified".
However, Dr Higginson cautioned that current efforts often focus on "quick and easy and cheap" measures, like diverting patients from A&E. He argued that sustainable solutions require:
- Making hospitals more efficient.
- Providing more staff for hospital beds.
- Dramatically improving community-based and social care to facilitate timely patient discharge.
He stressed that fixing the crisis is vital for staff welfare, many of whom are "run ragged, exhausted and suffering from a mixture of either burnout, moral injury or exhaustion [and] PTSD".
Official NHS England data for November shows 50,648 people waited over 12 hours in A&E from a decision to admit to actually being admitted. An NHS England spokesperson called this "totally unacceptable" and outlined winter plans involving productivity experts to drive down corridor care incidents.
The department spokesperson also pointed to some signs of recovery, noting that compared to last year, more patients are being seen within four hours and ambulance response times for serious conditions are faster.